Abstract
Rationale and Aim: In patients with Myeloma, early relapse following Autologous Haematopoietic Cell Transplantation (Auto-HCT) is a poor prognostic marker. Two groups have published scoring systems to predict early relapse. The CIBMTR score is based on cytogenetics, the bone marrow plasma cell percentage at the time of Auto-HCT and serum albumin. The GIMEMA Simplified early relapse in multiple myeloma (S-ERMM) score is a cumulative score based on a raised serum lactate dehydrogenase (LDH), t(4;14), del17p, low albumin, bone marrow plasma percentage >60%, and lambda light chain. The aim of the current study was to develop a scoring system to predict early relapse post-Auto-HSCT-1 using readily available variables.
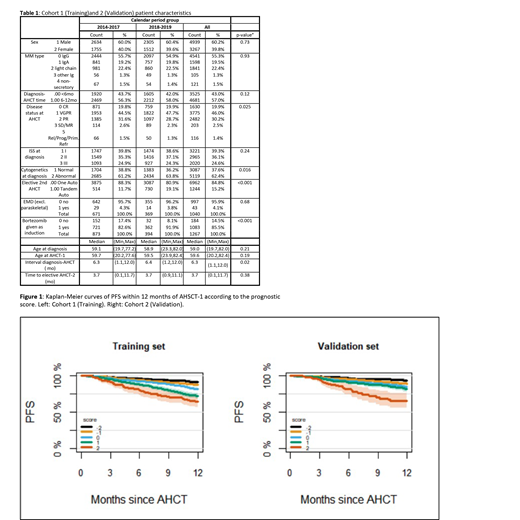
Study design and statistics: Within the EBMT database, there were 8,206 patients meeting the following eligibility criteria: First auto transplant 2014-2019, Known sex, ISS at diagnosis, cytogenetics analysis at diagnosis, disease status at Auto-HCT, Interval diagnosis-Auto-HCT > 1 month and <= 12 months, conditioning with Melphalan 200 mg/m2 and known information on relapse; tandem auto-allo patients were excluded. The analysis consisted of two steps: (1) Training: modeling based on 4,389 patients (611 events for PFS12) transplanted between 2014 and 2017, with internal validation carried out by bootstrapping; and (2) Testing: the models obtained were applied to 3,817 patients (346 events for PFS12) transplanted in 2018 and 2019 for external validation. The characteristics of the two cohorts are first reported separately and then together (Table 1). Possible adjustment factors analyzed for the prognostic model included Age at Auto-HCT, Known sex, ISS at diagnosis, disease status at Auto-HCT, and time from diagnosis to Auto-HCT. Complete cytogenetic information was not available at the time of this analysis and will be included in the later analysis. The shape of the effect of age and of time from diagnosis to Auto-HCT was investigated both by the analysis of residuals and by applying boot-strap backward selection among different alternatives. The final results were confirmed in a robustness analysis excluding patients undergoing tandem Auto-HCT.
Results: Comparison of the training and validation cohorts revealed no relevant differences (Table 1). Importantly, OS and PFS of both cohorts were overlapping with the probability of PFS at 12 months being 83.3% and 86.8%, respectively. The cumulative incidence of relapse at 12 month was 15.7% and 12.1%, respectively. Among patients who relapsed early, this occurred at a median of 6.64 months (0.56-11.99) in the first cohort, and at 5.85 months (0.1- 11.99) in the second cohort. The final model included (1) disease status at Auto-HCT, (2) age at Auto-HCT, and (3) ISS at diagnosis. Considering the order of magnitude of the coefficients, the points attributed in the risk score were: 0 for CR or VGPR; 1 for PR or SD/MR; 3 for Rel/Prog; 0 / 1/ 2 respectively for ISS I / II / III and -1 for Age<=55 yrs; -2 for Age (55-75 yrs]; -3 for Age>=75 yrs. The Hazard Ratio for a +1 point is 1.52 i.e. the risk of early relapse/death increased on average by 52% for each additional point in the score. The distribution of risk scores was as follows: Score= -2 (n=757), -1 (n=1,481), 0 (n=1,358), 1 (n=647), and 2 (n=146). The score allows separation of the PFS12 curves (Figure 1), with the lowest risk group (N=757) having a PFS at 12 months of 91%, and the highest risk group (N=146) having a PFS at 12 months of 65%. Despite some minor differences in the risk factors between the training and validation cohorts, the score has a similar average effect (HR=1.48 i.e. + 48% hazard for each additional point) and worked well in separating the curves, in particular in identifying the patients at high risk of early relapse.
Discussion and conclusion: The new EBMT score to predict early relapse post-Auto-HCT uses the easily available variables of age and ISS stage at diagnosis as well as the dynamic variable of response to induction. With this simple approach, we were able to clearly identify patients at high risk of early relapse. To our surprise, older age emerged as a protective factor against relapse. This may reflect a relative selection bias in that older patients with higher risk disease may not have been selected for transplant. Impact of cytogenetics will be presented at the Congress. In conclusion, this novel scoring system is robust and easy to use in routine daily practice.
Beksac: Amgen: Consultancy, Speakers Bureau; Janssen: Consultancy, Speakers Bureau; Celgene: Consultancy, Speakers Bureau; Sanofi: Consultancy, Speakers Bureau; Takeda: Consultancy, Speakers Bureau; Oncopeptides: Consultancy. Blaise: Jazz Pharmaceuticals: Honoraria. Leleu: Karyopharm Therapeutics: Honoraria; AbbVie: Honoraria; Bristol-Myers Squibb: Honoraria; Amgen: Honoraria; Merck: Honoraria; Mundipharma: Honoraria; Novartis: Honoraria; Carsgen Therapeutics Ltd: Honoraria; Oncopeptides: Honoraria; Janssen-Cilag: Honoraria; Gilead Sciences: Honoraria; Celgene: Honoraria; Pierre Fabre: Honoraria; Roche: Honoraria; Sanofi: Honoraria; Takeda: Honoraria, Other: Non-financial support. Forcade: Novartis: Consultancy, Other: Travel Support, Speakers Bureau; Gilead: Other: Travel Support, Speakers Bureau; Jazz: Other: Travel Support, Speakers Bureau; MSD: Other: Travel Support. Rabin: Janssen: Consultancy, Honoraria, Other: Travel support for meetings; BMS / Celgene: Consultancy, Honoraria, Other: Travel support for meetings; Takeda: Consultancy, Honoraria, Other: Travel support for meetings. Kobbe: Celgene: Research Funding. Sossa: Amgen: Research Funding. Hayden: Jansen, Takeda: Other: Travel, Accomodation, Expenses; Amgen: Honoraria. Schoenland: Pfizer: Honoraria; sanofi: Research Funding; janssen,Prothena,Takeda,: Consultancy, Honoraria. Yakoub-Agha: Jazz Pharmaceuticals: Honoraria.